
‘People travel for everything here’: Elliot Lake, Ont. offers affordable living, but also healthcare headaches for older adults
Northern Ontario city has the country’s third-highest concentration of people 65 and up

By Carly Penrose and Breanna Schnurr
Local News Data Hub
Feb. 7, 2024
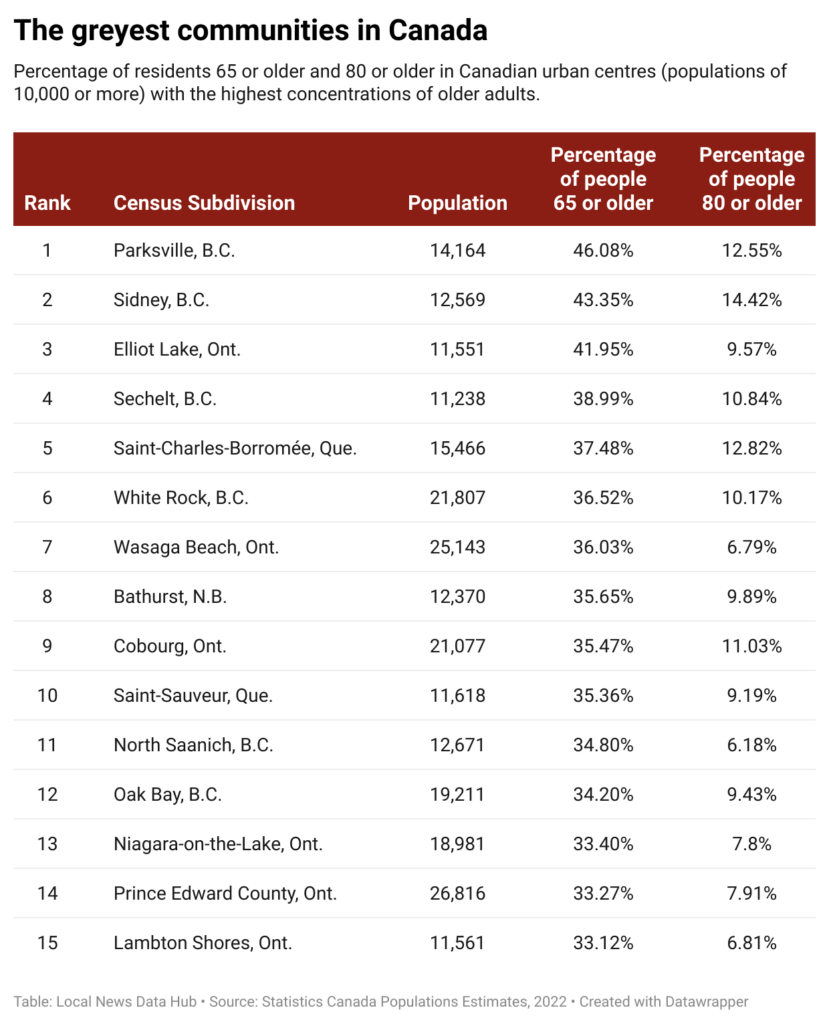
The golden years are not all golden in Elliot Lake, Ont., where people 65 or older make up 42 per cent of the population, more than in almost any other urban area in Canada.
Since the last uranium mine closed in 1996, the northern Ontario city of about 11,500 people has been marketing itself as a retirement destination with affordable housing and access to pristine nature.
These days, however, soaring dementia rates and health-care and transportation woes are also part of life in Elliot Lake, now home to the third highest concentration of older adults in the country, according to an analysis by the Local News Data Hub at Toronto Metropolitan University (TMU).
“If you have a really complicated medical situation… Elliot Lake is probably not for you,” said Marielle Brown, senior manager at Elliot Lake Retirement Living (ELRL), a not-for-profit housing corporation that helped lead the city’s rebranding effort.
Brown said she is upfront about the “trade-offs” involved in relocating to a more remote area when talking to prospective residents. “If they only stay six months, that doesn’t do me any good…I’m after people who stay as long as they can in their own home,” she said.
Elliot Lake isn’t the only municipality grappling with the challenges of an aging population. The Local News Data Hub’s analysis identified 111 urban centres in Canada where at least a quarter of residents are 65. The analysis, which ranked communities based on the percentage of older residents, focused on places with at least 10,000 people because that loosely aligns with what Statistics Canada considers the minimum population for an urban centre.
Dr. Samir Sinha, an internationally recognized geriatrician and director of health policy research at TMU’s National Institute on Aging, said the needs of older adults change over time.
“People tend to be able-bodied, healthy and independent in the first decade after retirement,” said Sinha, who is also director of geriatrics at University Health Network hospitals in Toronto.
Retired people, he added, may be drawn to more affordable communities or idyllic places. As they age, however, these same places can become “an absolute nightmare” in the absence of adequate health-care and other services.
Brown said Elliot Lake’s affordable housing is still a big draw. ELRL rents one-bedroom apartments for as low as $725 per month. House prices start at about $200,000.
Elliot Lake, however, is in the region covered by Algoma Public Health, where 8.6 per cent of people 65 or older do not have a family doctor. This compares to 5.9 per cent of older people nationwide, according to Statistics Canada data.
Marie Murphy-Foran, who lives in Elliot Lake and co-chairs the patient and family advisory council for the northeast Ontario health region, said local hospital services have expanded to include audiology, a visiting specialist program and some cancer treatments. But for the most part, “people travel for everything here.”
By way of example, Murphy-Foran said the knee replacement she required after a snowmobiling mishap involved multiple four-hour round-trips to Sudbury. Following the operation, she travelled 45 minutes each way to Blind River, Ont. for physiotherapy.
“I’m lucky because I have a husband [who drives], but a lot of people don’t,” Murphy-Foran said, noting that she couldn’t get behind the wheel of a car for six weeks after her surgery. The Ontario Northland bus service operates six days a week but it only runs once per day and turns the trip to Sudbury into a nearly three-hour trek.
Murphy-Foran, who is in her 70s, said Elliot Lake and communities like it are “perfect places to test some new, different [health-care] designs to meet the needs of the elderly.” For instance, the local clinic serving the nearby Serpent River First Nation offers free transportation for out-of-town medical appointments. In Elliot Lake, a similar program was deemed too costly, Murphy-Foran said.
Nationally, the share of Canada’s population that is 65 or older jumped to nearly 19 per cent in 2022, up from 14 per cent in 2010. That number is expected to stabilize around 25 per cent by the middle of the century.
The growing number of older Canadians poses additional challenges for municipalities facing what the Alzheimer Society of Canada says will be a “staggering” increase in dementia cases: In 2020, 8.4 per cent of Canadians over 65 had some form of dementia. By 2050, it is forecast to be 13.2 per cent.
Already in Elliot Lake roughly 13 per cent of the total population live with a cognitive impairment. “In a small community, I would say [that] is relatively high,” said Terry Caporossi, executive director of the Algoma Alzheimer Society.
Caporossi said the society’s Elliot Lake satellite office can’t keep up with the demand for service. The local branch offers community-based recreational therapy in town. Providing a real break for caregivers, however, is more challenging because the nearest adult day program is nearly 60 kilometres away in Blind River, Ont.
The Local News Data Hub used Statistics Canada’s 2022 population estimates to build the community ranking, which was reviewed by Sebastien Lavoie, a senior analyst at the Statistics Canada Centre for Demography. The analysis also found that:
- Just under 10 per cent of Elliot Lake residents are 80 or older. That compares to 4.5 per cent for Canada as a whole.
- The municipalities with the highest concentrations of residents 65 or older tend to be smaller — 87 of the 111 communities on the Local News Data Hub’s list have fewer than 30,000 residents.
- Two Vancouver Island communities topped the list. In first-ranked Parksville, B.C., 46 per cent of the 14,000 residents are older adults, while in second-place Sidney, B.C., they make up 43 per cent of the population.
- Doctor shortages are a reality for many of the municipalities with large cohorts of older adults. Statistics Canada data showed that in 2020, just under a third (33) of the 111 places on the Data Hub list were in health districts where at least 10 per cent of people 65 or older don’t have access to a family doctor.
- In addition to Elliot Lake, the list includes five other high-ranking Ontario communities. Wasaga Beach, where 36 per cent of residents are 65 or older, was seventh. In ninth-place Cobourg, older residents make up 35 per cent of the population. In Niagara-on-the-Lake, Prince Edward County, and Lambton Shores, which ranked 13th, 14th and 15th respectively, residents 65 or older make up about 33 per cent of the population.
Experts point to a variety of ways communities can be more age-friendly.
Sinha’s to-do list for local governments includes ensuring older residents can get around without a car. People outlive their decision to stop driving by 10 years on average, he noted. “How do they continue to get to the grocery store? How do they continue getting out to other activities and…connect with their friends and family?”
Sinha said age-friendly communities need public spaces with bathrooms and benches with armrests so it is easier to sit and get up.
Streets can also be made safer, he added, with changes such as extended crossing times at intersections. Statistics Canada data show that pedestrians over 70 are more than twice as likely to be killed in traffic incidents than pedestrians in any other age group.
International examples of age-friendly adaptations are also instructive. In Denmark, municipalities conduct home visits to identify older people needing care. In Singapore, families receive a housing grant for living near elderly relatives. France’s Paris Solidaire connects older adults with young people as roommates to share rent and provide companionship.
Closer to home, Vancouver International Airport offers sunflower lanyards to travellers with a cognitive impairment. This makes it easier for airport staff, who are trained in disability and dementia awareness, to identify and accommodate them.
The Alzheimer Society of New Brunswick, meanwhile, publishes guidelines for creating dementia-friendly indoor spaces that include using low-pattern carpeted floors because shiny floors can look wet and cause confusion.
This story was produced by the Local News Data Hub, a project of the Local News Research Project at Toronto Metropolitan University’s School of Journalism. The Canadian Press is the Data Hub’s operational partner. Detailed information on the data and methodology can be found here.